Clotting Cascade
The clotting cascade is a complex set of negative feedback mechanisms used by the human body as a means of maintaining blood haemostasis.How does the clotting cascade work? The process of coagulation occurs as a sequential results of a complex cascade involving platelets and numerous clotting factors (enzymes /proteins); however, there are three main pathways in which this system is activated. These include: the Tissue Factor Pathway (previously known as the extrinsic pathway), the Contact Activation Pathway (previously known as the intrinsic pathway) and the Common Pathway.
Understanding the clotting cascade is often the bane of any paramedical or medical student because of the number of clotting factors and pathways. A thorough understanding of the clotting cascade is important because it is with this knowledge that complex bleeding disorders and patients who have had a significant traumatic injury that medical staff and paramedics are able to combat the coagulopathy.
Clotting Cascade Factors
These are the main factors within the Clotting Cascade:
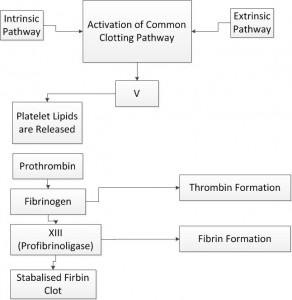
Initially triggered by either intrinsic or extrinsic release of chemical mediators that have triggered the Common Pathway (Factor X) to be released, the following clotting cascade occurs:
– I Fibrinogen
-II Prothrombin
– III Tissue Factor
– IV Calcium Ions
– V Ace Globulin
-VI Prothrombinase
– VII Antihaemophilic Factor A
-VIII Plasma Thromboplastin Component
– IX Stuart Factor
– X Antihaemophilic Factor C
-XI Hageman’s Factor
-XII Fibrin Stabilising Factor
This system has been described as the ” Clotting Cascade” effect because it works like a cascade, in which each phaze in the process initiates the release of the next clotting factor or clotting retraction factor. McCance & Huether (2002) acknowledge that ‘according to the cascade theory of coagulation each coagulation factors is converted into its active form by the preceeding factor until fibrin is produced’ (p.833).
The Tissue Factor Pathway (Extrinsic)
The Tissue Factor Pathway is the most prominent pathway involved in the clotting cascade and stimulates the release of the ‘Thrombin Burst’ in which thrombin is released. Thrombin circulates as a natural clotting factor in the normal healthy human circulatory system. When thrombin comes into contact with tissue factor (TF III) as a result of damage to collagen within the vasculature, the normally innate thrombin generates a ‘thrombin burst’ and commences the clotting cascade.
An example of the Tissue Factor Pathway/ Extrinsic pathway within the clotting cascade includes: when you cut yourself and this damages the collagen within the vasculature causing the contact of circulating thrombin with TFIII, which generates the commencement of the clotting cascade.
The Contact Activation Pathway (Intrinsic)
The Contact Activation Pathway (Intrinsic) is a much less common trigger for the clotting cascade and generally is not involved in haemostasis of normal, healthy individuals. The Contact Activation Pathway is activated during abnormal physiological parameters. Some of these pathophysiological conditions that may trigger the Contact Activation Pathway in the clotting cascade include: hyperlipidaemia, neutropenia/sepsis and any state of profound inflammation, which trigger the formation of a thrombus and thus activate the clotting cascade.
An example of the Contact Activation Pathway /Intrinsic pathway within the clotting cascade would be a patient who is suffering from Septic Shock and triggers the clotting cascade, which develops a clot and Disseminated Intravascular Coagulation (DIC) occurs. Please view my Disseminated Intravascular Coagulation Page for more information on DIC.
The Common Pathway (Final Pathway)
The Common Pathway can be triggered by either the Extrinsic or Intrinsic Pathway of the clotting cascade and result in the use of Thrombi to develop a haemostatic plug and activate many of the other factors within the clotting cascade. Following activation by the contact factor or tissue factor pathways, the coagulation cascade is maintained in a prothrombotic state by the continued activation of FVIII and FIX to form the tenase complex (clot), until normal haemostatic responses trigger the anticoagulant pathways. To learn more about the Anticoagulant Pathway, please review my Anticoagulant Pathway Page.
Virchow’s triad is clinically used to identify risks of thrombosis development in patients. Virchow’s Triad includes three broad categories of factors that are considered to contribute to thrombosis.
The Virchow’s triad consists of:
1. Alterations in normal blood flow
2. Injuries to the vascular endothelium
3. Alterations in the consistancy of blood (hypercoagulability)
To learn more about Virchow’s Triad please review my Virchow’s Triad page
